Angioplasty and Vascular Stenting
Angioplasty uses a balloon-tipped catheter to open a blocked blood vessel and improve blood flow. The doctor uses medical imaging, typically live x-rays, to guide the catheter across the blockage. Once the balloon spans the blockage, it is inflated to open the blocked vessel and improve blood flow. It may be done with or without a metal mesh tube called a stent. If a stent is used, it will be left inside the blood vessel to help keep it open.
Your doctor will tell you how to prepare and if you should take your regular medication. Angioplasty is minimally invasive and usually does not require general anesthesia. Most angioplasty procedures do not require an overnight stay. However, your doctor will discuss this with you. You may be told not to eat or drink anything several hours before the procedure. Tell your doctor if there's a chance you are pregnant. List any recent illnesses, medical conditions, allergies and medications you're taking. Leave jewelry at home and wear loose, comfortable clothing. You may need to change into a gown for the procedure.
- What are Angioplasty and Vascular Stenting?
- What are some common uses of the procedures?
- How should I prepare?
- What does the equipment look like?
- How does the procedure work?
- How is the procedure performed?
- What will I experience during and after the procedure?
- Who interprets the results and how do I get them?
- What are the benefits vs. risks?
- What are the limitations of Angioplasty and Vascular Stenting?
What are Angioplasty and Vascular Stenting?
Angioplasty, with or without vascular stenting, is a minimally invasive procedure. It is used to improve blood flow when a vein or artery is too narrow or blocked. It is usually done in an interventional radiology suite rather than operating room.
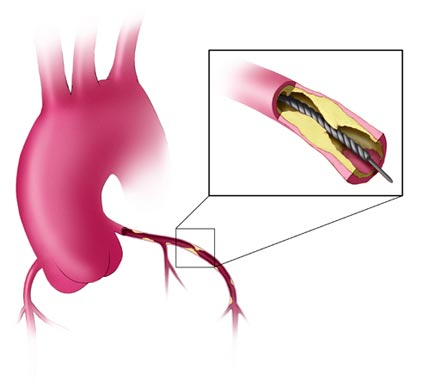
In angioplasty, x-ray fluoroscopy or other imaging is used to guide a balloon-tipped catheter (a long, thin plastic tube) into an artery or vein to where it is narrowed or blocked. The balloon is inflated to open the vessel, then deflated and removed.
A metal mesh tube called a stent may be permanently placed in the newly opened vessel to help keep it open. There are different types of stents, including wire mesh. Stents covered in fabric-type material are called stent grafts.
What are some common uses of the procedures?
Angioplasty with or without stenting is commonly used to treat conditions that narrow or block blood vessels and interrupt blood flow. These conditions include:
- coronary artery disease, a narrowing of the arteries that carry blood and oxygen to the heart muscle.
- narrowing of the large arteries due to hardening of the arteries or atherosclerosis. This is a build-up of cholesterol and other fatty deposits, called plaques, on the artery walls.
- peripheral artery disease (PAD), a narrowing of the arteries in the legs or arms.
- carotid artery stenosis, a narrowing of the neck arteries supplying blood to the brain.
- narrowing or blockage in the veins in the chest, abdomen, pelvis, arms and legs.
- renal vascular hypertension, high blood pressure caused by a narrowing of the kidney arteries. Angioplasty and stenting may be used to help improve kidney function.
- narrowing in dialysis fistula or grafts. Fistulas and grafts are artificial blood vessel connections doctors use in kidney dialysis. Angioplasty is generally used when these connections become narrow or blocked. Stenting may also be needed in some cases. See the Dialysis and Fistula/Graft Declotting and Interventions page for more information.
How should I prepare?
Tell your doctor about all the medications you take, including herbal supplements. List any allergies, especially to local anesthetic, general anesthesia, or contrast materials. Your doctor may tell you to stop taking aspirin, nonsteroidal anti-inflammatory drugs (NSAIDs) or blood thinners before your procedure.
Tell your doctor about recent illnesses or other medical conditions.
Women should always tell their doctor and technologist if they are pregnant. Doctors will not perform many tests during pregnancy to avoid exposing the fetus to radiation. If an x-ray is necessary, the doctor will take precautions to minimize radiation exposure to the baby. See the Radiation Safety page for more information about pregnancy and x-rays.
In most cases, you should take your usual medications, especially blood pressure medications. Take these with sips of water on the morning of your procedure.
Other than medications, your doctor may tell you to not eat or drink anything for several hours before your procedure.
You may need to stay overnight at the hospital.
What does the equipment look like?
In these procedures, x-ray imaging equipment, a balloon catheter, sheath, stent and guide wire are used.
This exam typically uses a radiographic table, one or two x-ray tubes, and a video monitor. Fluoroscopy converts x-rays into video images. Doctors use it to watch and guide procedures. The x-ray machine and a detector suspended over the exam table produce the video.
A guide wire is a thin wire used to guide the placement of the diagnostic catheter, angioplasty balloon catheter and the vascular stent. A sheath is a vascular tube placed into the access artery, such as the femoral artery in the groin.
A balloon catheter is a long, thin plastic tube with a tiny balloon at its tip. A stent is a small, metal mesh tube. Balloons and stents come in different sizes to match the size of the diseased artery.
Stents are specially designed mesh, metal tubes that are inserted into a blood vessel in a collapsed state on a catheter. They are expanded inside the vessel to prop the walls open. In some cases, a stent may have a synthetic fabric covering.
This procedure may use other equipment, including an intravenous line (IV), ultrasound machine and devices that monitor your heart beat and blood pressure.
How does the procedure work?
Using image guidance, the doctor inserts the balloon catheter through the skin into an artery. They advance the balloon across the site of the blockage where it is inflated to open the vessel. The doctor deflates the balloon once the vessel is open. In this process, the balloon expands the artery wall, increasing blood flow through the artery. The doctor may place a stent at the treatment site to hold the artery open.
How is the procedure performed?
Angioplasty and stenting should only be performed by a doctor specially trained in these minimally invasive techniques.
You will lie on the procedure table.
The doctor or nurse may connect you to monitors that track your heart rate, blood pressure, oxygen level, and pulse.
A nurse or technologist will insert an intravenous (IV) line into a vein in your hand or arm to administer a sedative. This procedure may use moderate sedation. It does not require a breathing tube. However, some patients may require general anesthesia.
The nurse will sterilize the area of your body where the catheter is to be inserted. They will sterilize and cover this area with a surgical drape.
Your doctor will numb the area with a local anesthetic. This may briefly burn or sting before the area becomes numb.
The doctor will make a very small skin incision at the site.
A sheath is first inserted into the blood vessel.
Guided by live x-rays, the doctor inserts the catheter through the skin and guides it through the blood vessels until it reaches the blockage. Once the catheter is in place, contrast material will be injected into the artery to perform an angiogram. An angiogram is an x-ray picture of the inside of the blood vessels. This will help identify where the blockage is.
Using x-ray guidance, the doctor crosses the narrowing or blockage with a guide wire. This allows the balloon-tipped catheter to pass over the wire. Once across the blockage, the balloon will be inflated for a short time. Sometimes the balloon needs to be inflated more than once. Or, other blood vessels need to be treated during the same procedure.
More x-rays are taken to see how much blood flow has improved. The balloon catheter, wire, and sheath will be removed.
Many times, stents need to be permanently placed inside the blood vessel to help keep it open. Some stents can open on their own. Others need a balloon to open. Balloon stents are typically expanded against the blood vessel wall. When the balloon is deflated and removed, the stent remains. The permanent stent acts like a scaffold for the artery. Drug-coated stents have been approved for use by the U.S. Food and Drug Administration (FDA). The drug is slowly released to help keep the blood vessel from narrowing again. This is a condition called restenosis.
Drug-coated balloons may also be used for patients with PAD or dialysis fistulas. When the balloon is inflated, the drug enters the wall of the blood vessel. It stays there for some time even after the balloon has been removed.
When the procedure is complete, the doctor will remove the catheter and apply pressure to stop any bleeding. Sometimes, your doctor may use a closure device to seal the small hole in the artery. This will allow you to move around more quickly. No stitches are visible on the skin. The nurse will cover this tiny opening in the skin with a dressing.
You may need to lie in bed with your legs straight for several hours. When an arm or wrist was used for access, you may have activity restrictions to follow.
When the procedure is done, you will be transferred to a recovery room or to a hospital room.
The doctor or nurse will remove your IV line before you go home.
Talk to your doctor about how long the procedure will take.
This procedure is often done on an outpatient basis. However, some patients may require admission following the procedure. Ask your doctor if you will need to be admitted.
What will I experience during and after the procedure?
The doctor or nurse will attach devices to your body to monitor your heart rate and blood pressure.
You will feel a slight pinch when the nurse inserts the needle into your vein for the IV line and when they inject the local anesthetic. Most of the sensation is at the skin incision site. The doctor will numb this area using local anesthetic. You may feel pressure when the doctor inserts the catheter into the vein or artery. However, you will not feel serious discomfort.
If the procedure uses sedation, you will feel relaxed, sleepy, and comfortable. You may or may not remain awake, depending on how deeply you are sedated.
You may feel slight pressure when the doctor inserts the catheter, but no serious discomfort.
As the contrast material passes through your body, you may feel warm. This will quickly pass.
It is common for patients to feel some mild discomfort when the balloon is inflated. This is because the artery is being stretched. Discomfort is more noticeable when veins are opened or dilated. This discomfort should decrease as the balloon is deflated.
The site where the catheter was inserted may be bruised and sore. This is temporary and resolves in a few days.
Your blood pressure and heart rate will be monitored for several hours. Your catheter site will be checked for bleeding or swelling, too. Bleeding at the site where the catheter entered the vein when veins are treated is less likely. Therefore, you may be discharged earlier if the procedure is performed for vein disease such as dialysis fistula. Your doctor may prescribe medicine to relax your arteries, protect against artery spasm and prevent blood clots.
If contrast material was used, your body will get rid of it during urination. Your urine will not be discolored. You may be asked to drink extra fluids to help flush out the contrast material.
At home, you should rest and drink plenty of fluids. Avoid lifting heavy objects and strenuous exercise for at least 24 hours. You should avoid smoking permanently. Smoking is a major cause of atherosclerosis. If bleeding begins where the catheter was inserted, you should lie down. Apply pressure to the site and call your doctor. Tell your doctor right away if your leg changes color or if you feel pain or warm where the catheter was inserted.
After the procedure, you may be prescribed aspirin or blood thinners. These drugs can prevent blood clots from forming. Your doctor will monitor the effect of some medicines with frequent blood tests.
Magnetic resonance imaging (MRI) can probably be done right after stenting. However, make sure you tell the MRI department that you have a stent. Today's stents are considered safe for MRI, but you may need several weeks after stenting for MRI to be safe. Metal detectors do not affect a stent. Your doctor may give you a card with stent information. Keep it in your wallet. Show this to the MRI department to help determine safety.
Who interprets the results and how do I get them?
The interventional radiologist can tell you whether the procedure was a success by comparing your before and after angiograms.
Your interventional radiologist may recommend a follow-up visit.
This visit may include a physical check-up, imaging exam(s), and blood tests. During your follow-up visit, tell your doctor if you have noticed any side effects or changes.
What are the benefits vs. risks?
Benefits
- Compared to bypass surgery, balloon angioplasty and stent placement are much less invasive and relatively low-risk, low-cost procedures.
- These procedures are performed using local anesthesia. Because general anesthetic is not required in most patients, there is no extended stay in the hospital.
- No surgical incision is necessary—only a small nick in the skin that does not need stitches.
- You will be able to return to your normal activities shortly afterwards.
Risks
- Major complications after angioplasty are rare. However, inserting the catheter may injure the artery. There is also a very small risk of blood clots or tearing the artery.
- When angioplasty is done alone, blockages can recur. Most of these arteries can be opened again successfully. This can also occur when a stent is placed in the artery at the time of the angioplasty.
- Heavy bleeding from the catheter insertion site may require special medication or a blood transfusion.
- There is a risk of stroke when angioplasty and/or stenting are performed on the carotid artery.
- A rare complication associated with angioplasty is abrupt vessel closure. This blockage in the treated area typically occurs within 24 hours of the procedure. If it happens, medication to dissolve clots followed by angioplasty or stenting may be used. In some cases, emergency bypass surgery may be needed.
- Other rare complications include heart attack and sudden cardiac death.
- Any procedure where the skin is penetrated carries a risk of infection.
- There is a very slight risk of an allergic reaction if the procedure uses an injection of contrast material.
- Any procedure that places a catheter inside a blood vessel carries certain risks. These risks include damage to the blood vessel, bruising or bleeding at the puncture site, and infection. The doctor will take precautions to mitigate these risks.
- Contrast material may cause a decrease in kidney function, particularly if it already exists. Your doctor will check your kidney function before the procedure in order to lower this risk. See the Contrast Materials page for more information.
What are the limitations of Angioplasty and Vascular Stenting?
Angioplasty with vascular stenting is just one way to treat narrowed or blocked arteries. Medication and exercise are often the first step.
Angioplasty does not reverse or cure the underlying disease of atherosclerosis. It is very important for patients to make lifestyle changes, including eating a healthy diet that is low in saturated fat, exercising and not smoking. Patients with diabetes, high blood pressure and/or high cholesterol need to follow the treatment plan prescribed by their doctors.
Angioplasty may have to be repeated if the same artery becomes blocked again, a condition called restenosis. If a stent is placed, the chance of restenosis is reduced but it can still occur.
Only about half of patients with renal vascular hypertension caused by atherosclerosis have their blood pressure successfully treated or improved by angioplasty/stenting. By the time it is done, many of these patients have disease in small arteries within the kidney that does not respond to angioplasty.
Angioplasty and vascular stenting for peripheral artery disease (PAD) affecting arteries in the pelvis and legs is less successful when multiple leg vessels are narrowed or when small vessels have to be opened. Patients with PAD can benefit from quitting smoking, proper diet, regular exercise and controlling blood cholesterol.
Carotid artery angioplasty and stenting is approved by the FDA. A dedicated filter device may be used during stenting to help keep blood clots and other plaques from passing into the brain. This helps lower the risk of stroke. Surgical repair has been done for many years. It has been proven effective and safe when done by skilled surgeons. Talk to your doctor about the risks and benefits of carotid artery stenting.
Additional Information and Resources
American Stroke Association: www.strokeassociation.org
National Stroke Association: www.stroke.org
Society of Interventional Radiology (SIR) - Patient Center
This page was reviewed on June 01, 2022